By THE NEW YORK TIMES
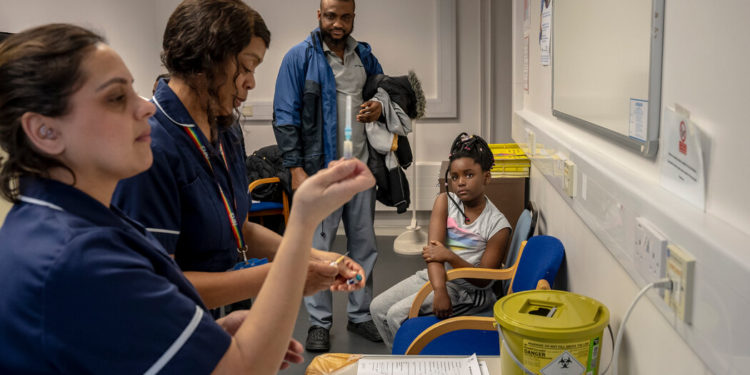
The 5-year-old looked nervously at her older brothers, scanning their faces for any sign of distress as needles were swiftly stuck into their upper arms, the syringe plungers pushed in and the measles, mumps and rubella vaccine administered. Whether it was for her benefit or not, they barely flinched.
Then it was her turn. The girl, Oma Nnagbo, looked wide-eyed at the cheerful nurse who a moment later declared, “All done, very brave!”
Michael Nnagbo, 40, had brought his three children to this pop-up vaccine clinic in Wolverhampton in England’s West Midlands after receiving a notice from their school about a measles outbreak in the nearby Birmingham area.
“It’s what we have to do, and it’s important to do,” Mr. Nnagbo said. “I just want them to be safe. And it was easy, you could just walk in.”
Cases of measles, a highly contagious but easily preventable disease, have begun to crop up in clusters as the number of children getting the combined measles, mumps and rubella vaccine has declined globally. The trend worsened after the coronavirus pandemic because of a lack of access and hesitancy among some groups. The measles virus can cause serious illness and, in the most extreme cases, death.
Across Europe, measles cases rose more than 40-fold in 2023 compared with a year earlier — from less than 1,000 to more than 40,000 — according to the World Health Organization. And while much of that increase was concentrated in lower-income nations like Kazakhstan, more prosperous nations, where higher vaccination rates had long made cases measles rare, are also experiencing worrying outbreaks.
In Britain, 650 cases of measles were confirmed between Oct. 1 and the end of February, according to the U.K. Health Security Agency, which declared a national incident in January. The rise in cases was initially driven by an outbreak in the West Midlands, but it has spread elsewhere around the country. Most of the cases in Britain are in children under 10.
Vaccine coverage has waned to precarious rates in some communities, particularly those facing the highest levels of deprivation. That was less the result of a surging anti-vaccine movement, experts said, than a lack of resources, lack of awareness, and some culturally driven hesitancy.
The percentage of children being immunized through the country’s routine vaccination program has fallen over the past decade across all illnesses, including whooping cough, measles, mumps and rubella, polio, meningitis and diphtheria.
England no longer has the levels of vaccine coverage recommended by the World Health Organization, which advises that more than 95 percent of people must have had two doses of a measles vaccine that contains weakened amounts of the virus to prevent outbreaks.
England had 84.5 percent measles vaccine coverage by the end of 2023, but in some areas it was far lower. London had a coverage rate of 73.1 percent overall, even lower than the West Midlands, where the coverage was 83.6 percent at the end of last year.
Jenny Harries, the chief executive of health security agency, said in a statement that the lower vaccine rates were linked to inequality.
“While the majority of the country is protected, there are still high numbers of children in some areas that continue to be unprotected from preventable diseases,” she said. “Unless uptake improves we will start to see the diseases that these vaccines protect against re-emerging and causing more serious illness.”
Carol Dezateux, a professor of pediatric epidemiology at Queen Mary University of London, said the current measles outbreak was “entirely predictable,” as immunizations had fallen to alarmingly low levels even before the pandemic. The causes were complex, she said, but the lockdowns and worries about exposure to the coronavirus made the problem worse.
Vaccination rates for children in England have been steadily declining over the last decade, partly because of vaccine hesitancy but also because of a lack of resources and logistical issues in the most deprived areas. It’s not just the M.M.R. vaccine, Dr. Dezateux said, as there is evidence of widening inequalities between wealthy and poor children across Britain in all five of the key childhood vaccinations.
“There’s a failure to think about how we can move the dial on this,” in a more coordinated way, Dr. Dezateux said, adding, “You might like to climb a high mountain, but if you’ve got no prospect of even getting up to the first base camp, you’re never going to try it, you know?”
The coverage gap has been difficult to close in some areas, Dr. Dezateux said, because so much pressure has fallen onto general practitioners in the country’s National Health Service who are already severely stretched.
Still, the cost of prevention in the form of vaccines is about 4 percent of the cost of an outbreak, she said, showing the need for a cohesive and coordinated plan to work toward better vaccine uptake.
“We know that where resources are brought in, then people can do more. It’s not rocket science,” Dr. Dezateux said.
Dr. Milena Marszalek, a research fellow at Queen Mary who is a general practitioner in northeast London in an area that has one of the country’s worst vaccination rates, said it was a logistical struggle to combat dropping vaccine coverage.
“There is a real problem with lack of capacity, lack of appointments,” she said. “We haven’t got the resources needed to bring the kids in for vaccination.”
Still, some things worked, she said, citing pop-up clinics and outreach with local imams to relay information about the safety of the vaccine to the large Muslim South Asian community in the area.
Local Haredi Jewish families told her that flexible hours at clinics and walk-in appointments also removed a barrier.
Still, it is often only after a significant outbreak that the issue of vaccination takes on greater urgency. Nicole Miles, the lead nurse for Vaccination UK, a group commissioned by Britain’s National Health Service to deliver childhood vaccines and who ran the Wolverhampton clinic, said that an accessible, sensitive and tailored approach was important.
“What people don’t realize is how sick it makes you,” Ms. Miles said of the measles virus. “There is this idea that, ‘Well it’s just measles,’ because we haven’t seen cases of measles for years like we are now. So people don’t realize how dangerous it can be, since it just hasn’t been here.”
Ms. Miles, 34, and two other nurses who were working to distribute the vaccines discussed how vaccine hesitancy among their patients was actually quite rare.
“There are always going to be cohorts of people who don’t want to be vaccinated,” Ms. Miles said. “And essentially, there’s nothing we can do about that, is there? But we need to vaccinate the people who do want to be vaccinated and who have been missed along the line somehow.”
At the Wolverhampton clinic, many of the families coming in said that they were not opposed but had not gotten vaccinations for one reason or another. Like Mr. Nnago, many had heard about the vaccination push through schools.
The Okusanya family, originally from Nigeria, has been living in Wolverhampton for two years. Oluwafunmilayo Okusanya, 42, said none of her three children had received the M.M.R. vaccine in their home country, so when she heard of the measles outbreak locally, she knew it was important to bring them in.
“When the opportunity came, I felt it was a good thing for them to have it,” she said. “It’s made it very convenient. Although some might not see the need to come around for it, we just need to protect the kids.”






Discussion about this post